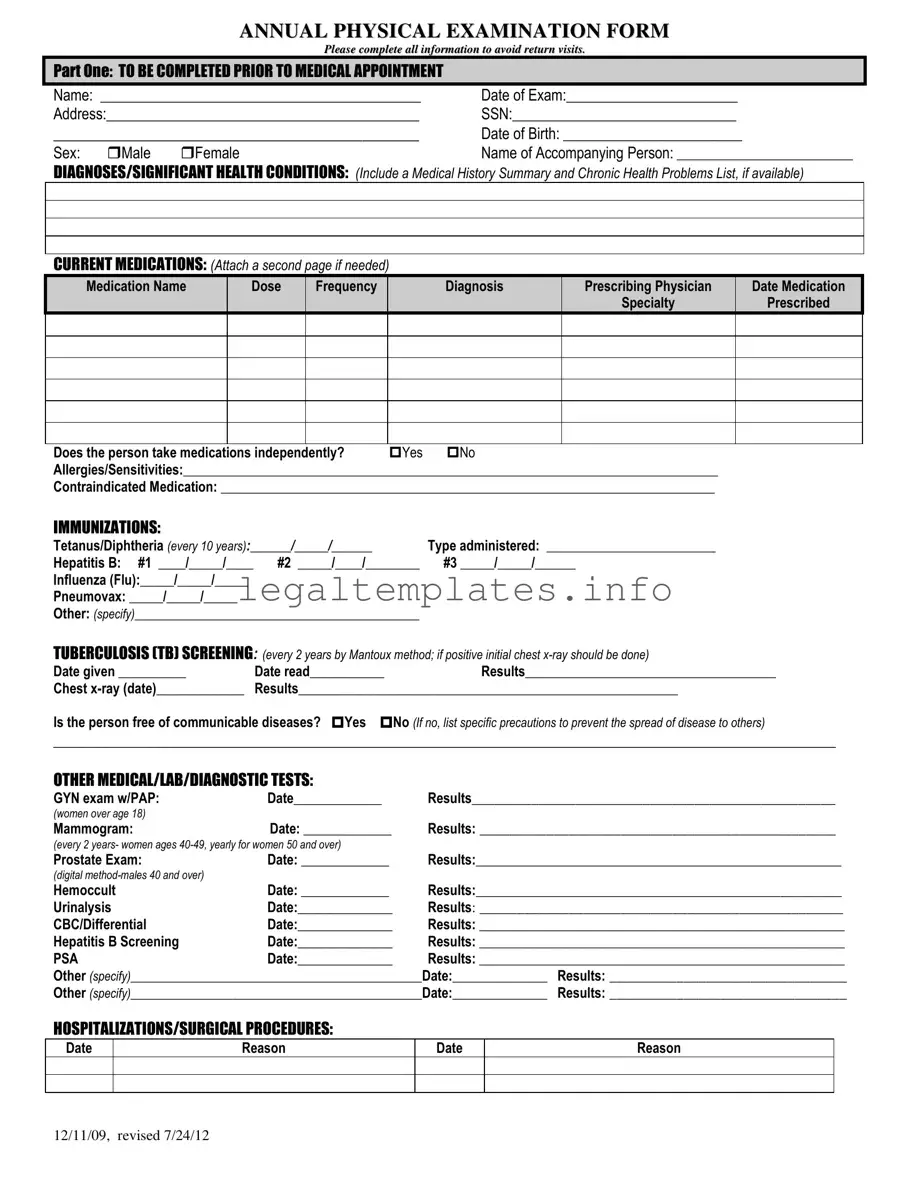
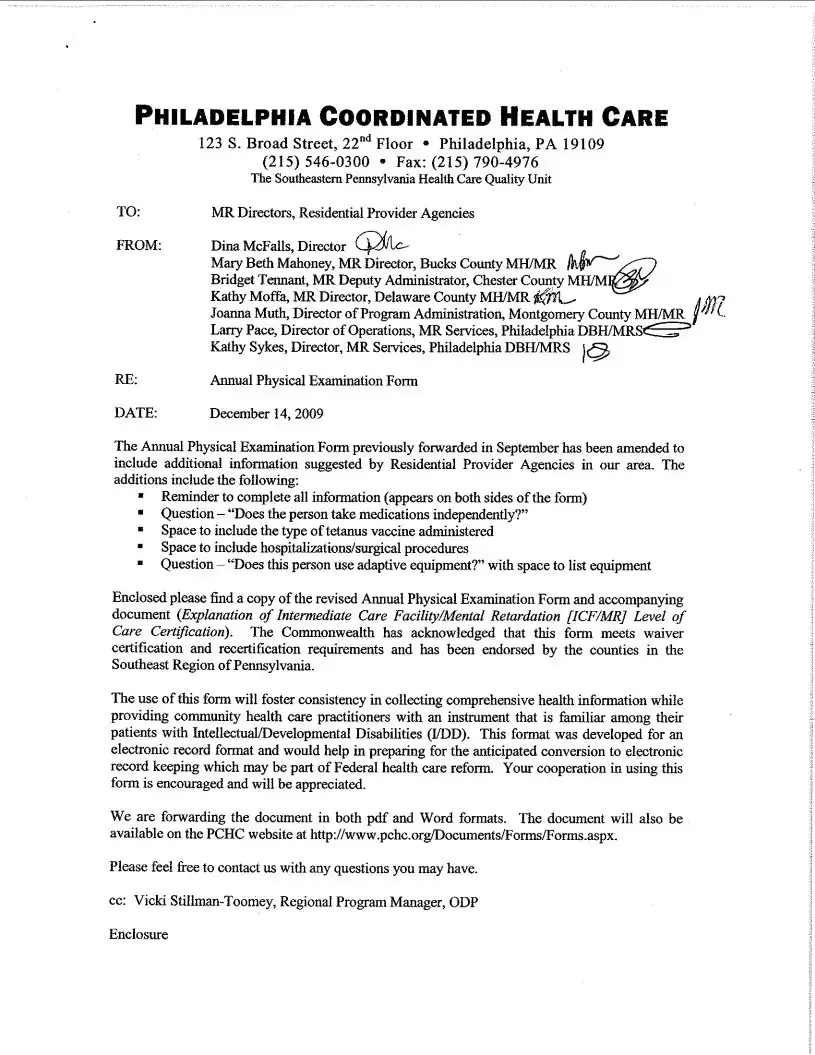
What is the purpose of the Annual Physical Examination form?
The purpose of the Annual Physical Examination form is to provide a comprehensive overview of an individual's current health status. It gathers detailed information about the patient's medical history, diagnoses, medications, immunizations, and results from various medical, lab, and diagnostic tests. It aims to identify any health issues early on, track any changes in the patient's health over time, and help in the planning of medical care. Completing this form thoroughly ensures that healthcare providers have all the necessary information to offer the best possible care, and helps to avoid unnecessary return visits.
Why do I need to complete all the information on the form?
Completing all the information on the form is crucial because it provides your healthcare provider with a full picture of your health. This includes your medical history, current medications, immunizations, and recent tests or procedures, among other details. Accurate and comprehensive information helps in making informed decisions about your care, identifying any potential health issues early, and ensuring that your healthcare plan is up-to-date. It also prevents the need for follow-up visits to collect missing information, saving you time and helping to manage your health more efficiently.
Can I attach additional pages if there’s not enough space for my medications?
Yes, you are encouraged to attach additional pages if the space provided for listing your current medications is not sufficient. It's important to include detailed information about each medication, such as the name, dosage, frequency of intake, the diagnosis for which it was prescribed, the prescribing physician, and the date it was prescribed. Providing a complete list of medications, including any over-the-counter drugs or supplements you're taking, ensures that your healthcare provider has a comprehensive understanding of your treatment regimen.
What should I do if I don’t have all the required information for the form?
If you find that you do not have all the required information to complete the form, it's important to gather as much of it as possible before your appointment. You may need to contact previous healthcare providers for records of immunizations, past medical tests, or procedures. If there are sections you cannot complete, inform your current healthcare provider at the time of your appointment. They can help you determine the best course of action, whether it involves setting up follow-up tests or obtaining records from other sources.
Is the Annual Physical Examination form confidential?
Yes, the Annual Physical Examination form, like all medical records, is confidential. The information you provide is protected under patient privacy laws, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States. This means that your personal and medical information cannot be disclosed to anyone except as necessary for your medical care or as required by law, without your explicit consent.
How often do I need to fill out the Annual Physical Examination form?
The Annual Physical Examination form is intended to be completed once every year. This yearly health checkup helps in monitoring your health over time, identifying any new or potential health issues, and updating your medical care plan accordingly. It is an essential part of preventative healthcare and ensures that you and your healthcare provider are aware of any changes in your health status.
What happens if my health status changes after I've submitted the form?
If your health status changes after you've submitted the form, it's important to inform your healthcare provider as soon as possible. This can include new diagnoses, changes in medication, or other significant health changes. Keeping your healthcare provider informed allows them to offer the most accurate and appropriate care based on your current health needs.