Fill a Valid Certification Of Incapacity Form
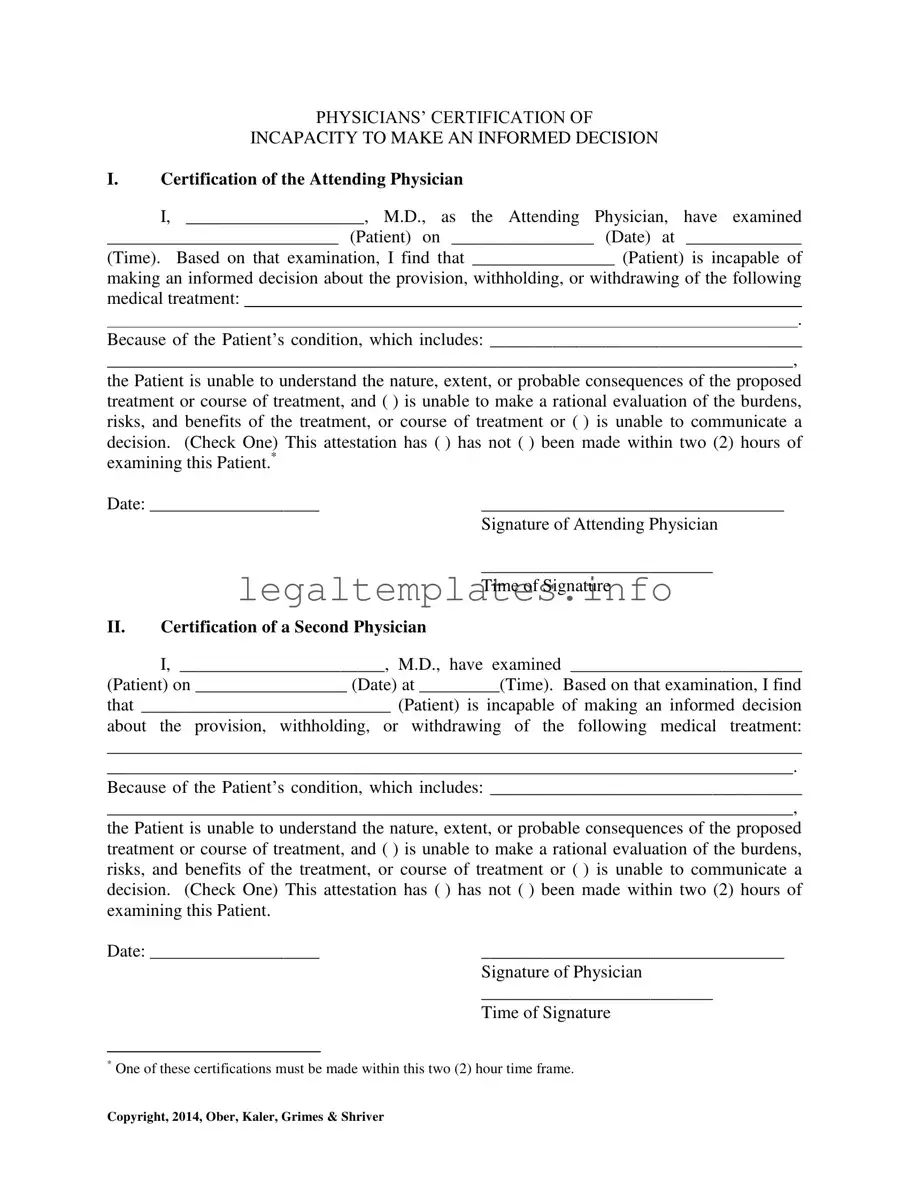
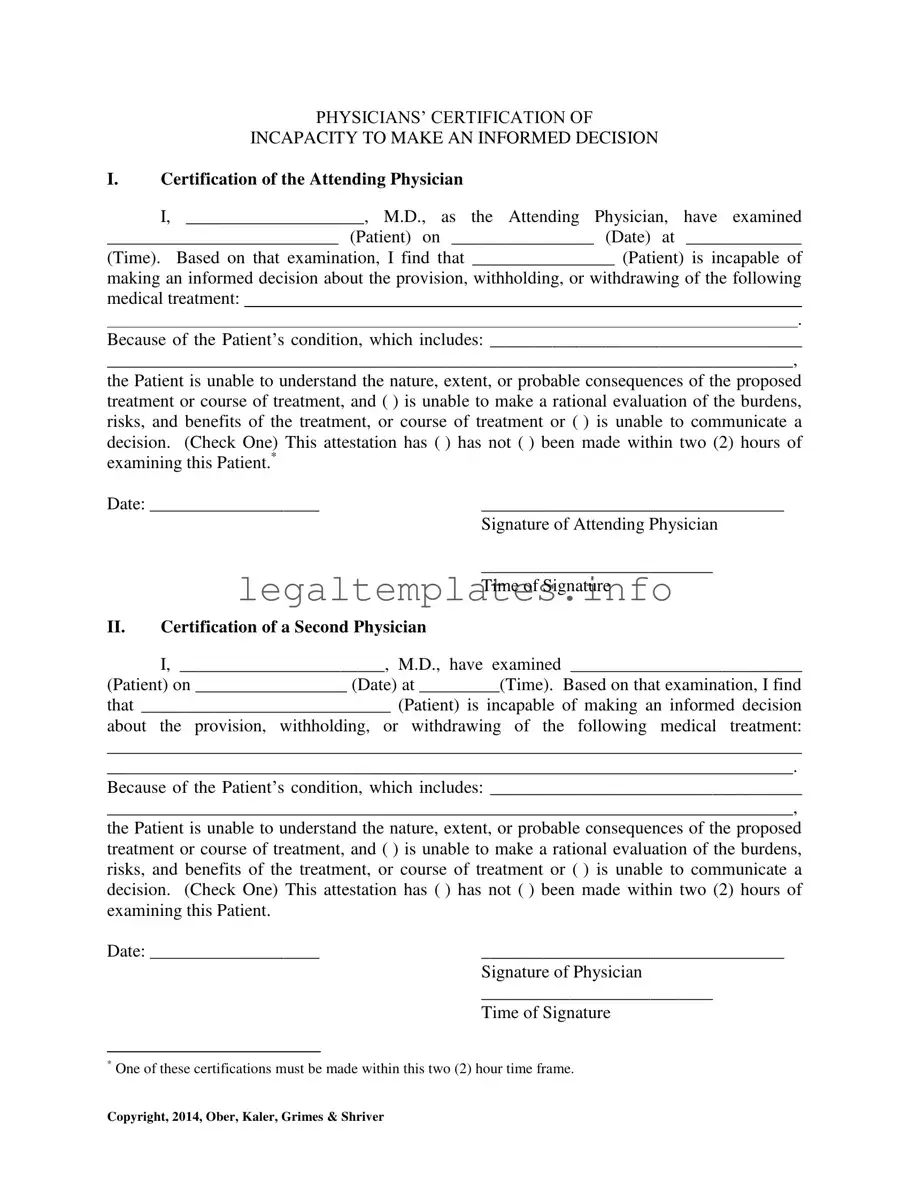
The Certification of Incapacity form is a crucial document completed by physicians to verify that a patient is unable to make an informed decision regarding their medical treatment. This form includes the physicians' observation and detailed assessment of the patient's condition, confirming that the patient cannot comprehend the nature, extent, or probable consequences of the proposed medical treatment. If you or a loved one need to understand the importance of this form or are preparing to fill it out, click the button below for more information.
Access Certification Of Incapacity Online
Fill a Valid Certification Of Incapacity Form
Access Certification Of Incapacity Online
Access Certification Of Incapacity Online
or
Click for PDF Form
This form won’t take long
Edit, save, and complete Certification Of Incapacity online.
