Skin Monitoring: Comprehensive CNA Shower Review
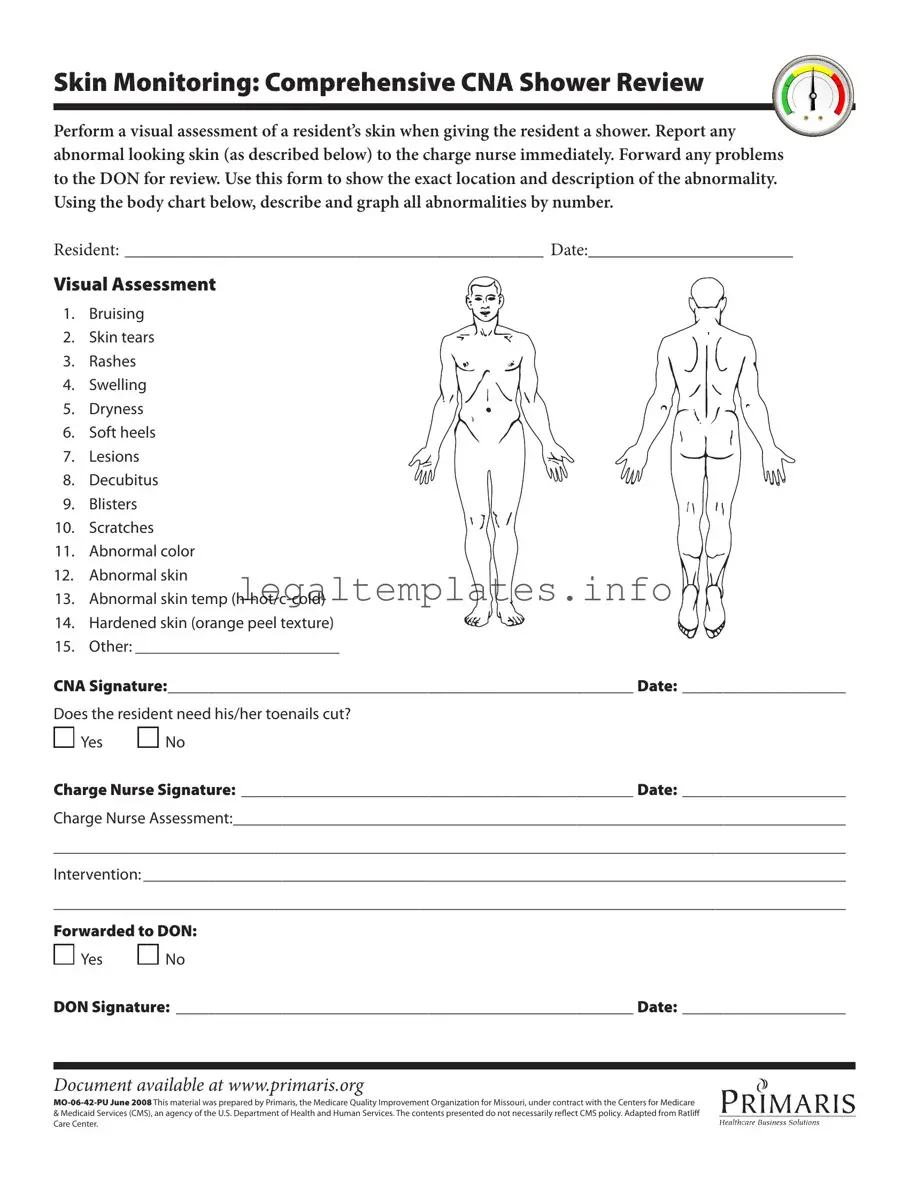
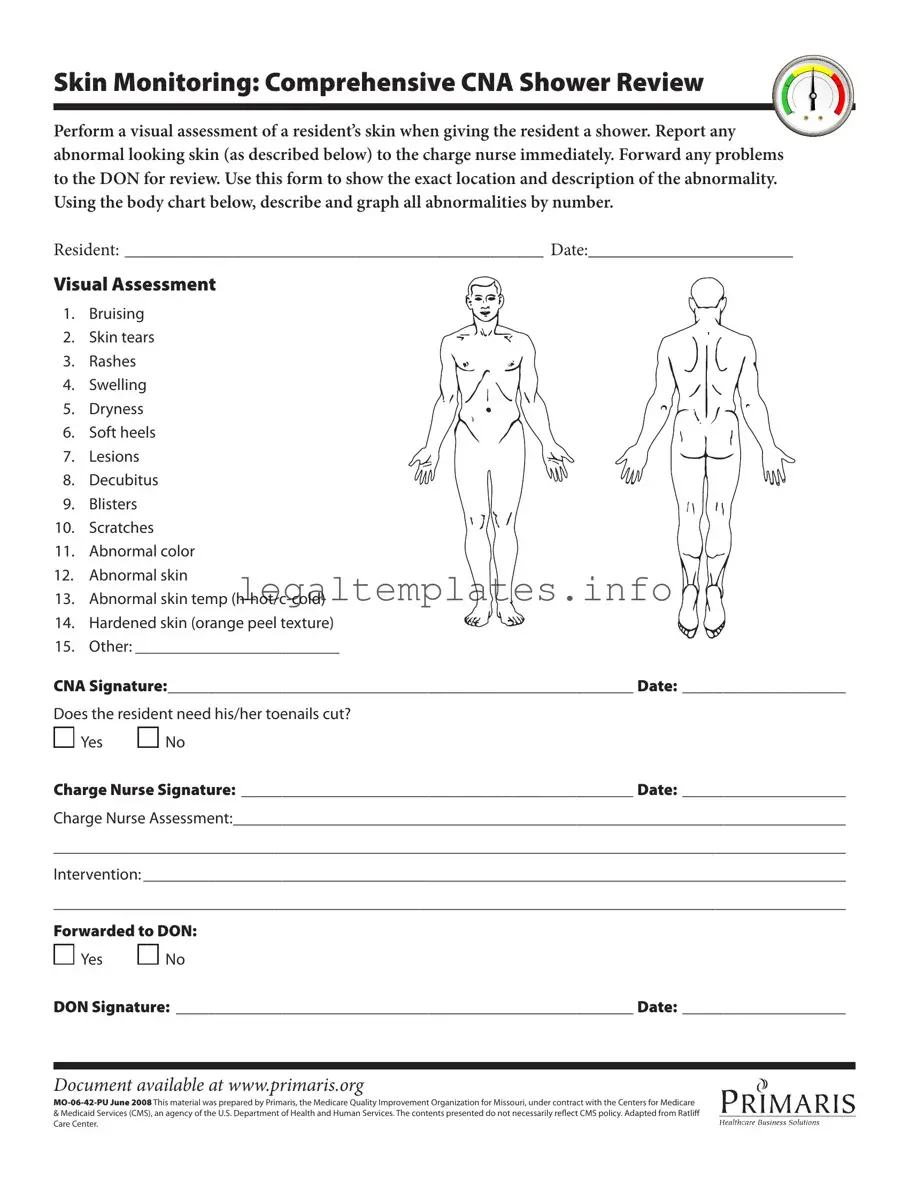
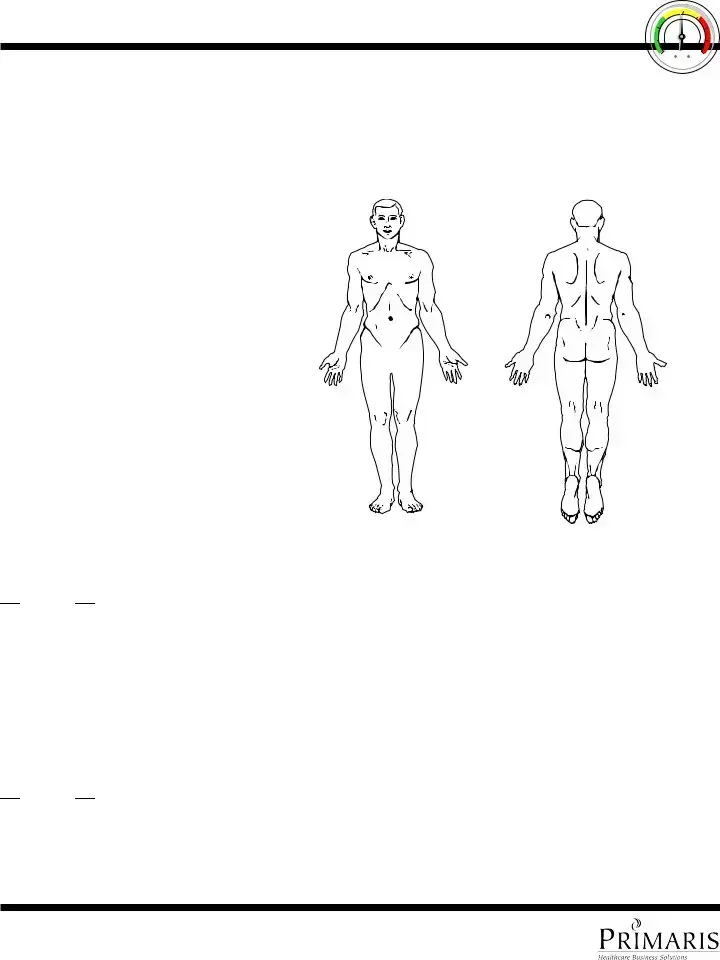
Perform a visual assessment of a resident’s skin when giving the resident a shower. Report any abnormal looking skin (as described below) to the charge nurse immediately. Forward any problems to the DON for review. Use this form to show the exact location and description of the abnormality. Using the body chart below, describe and graph all abnormalities by number.
RESIDENT: _______________________________________________ DATE:_______________________
Visual Assessment
1. Bruising
2. Skin tears
3. Rashes
4. Swelling
5. Dryness
6. Soft heels
7. Lesions
8. Decubitus
9. Blisters
10. Scratches
11. Abnormal color
12. Abnormal skin
13. Abnormal skin temp (h-hot/c-cold)
14. Hardened skin (orange peel texture)
15. Other: _________________________
CNA Signature:_________________________________________________________ Date: ____________________
Does the resident need his/her toenails cut?

 Yes
Yes 
 No
No
Charge Nurse Signature: ________________________________________________ Date: ____________________
Charge Nurse Assessment:___________________________________________________________________________
_________________________________________________________________________________________________
Intervention: ______________________________________________________________________________________
_________________________________________________________________________________________________
Forwarded to DON:

 Yes
Yes 
 No
No
DON Signature: ________________________________________________________ Date: ____________________
Document available at www.primaris.org
MO-06-42-PU June 2008 This material was prepared by Primaris, the Medicare Quality Improvement Organization for Missouri, under contract with the Centers for Medicare
&Medicaid Services (CMS), an agency of the U.S. Department of Health and Human Services. The contents presented do not necessarily relect CMS policy. Adapted from Ratlif Care Center.

 Yes
Yes 
 No
No
 Yes
Yes 
 No
No