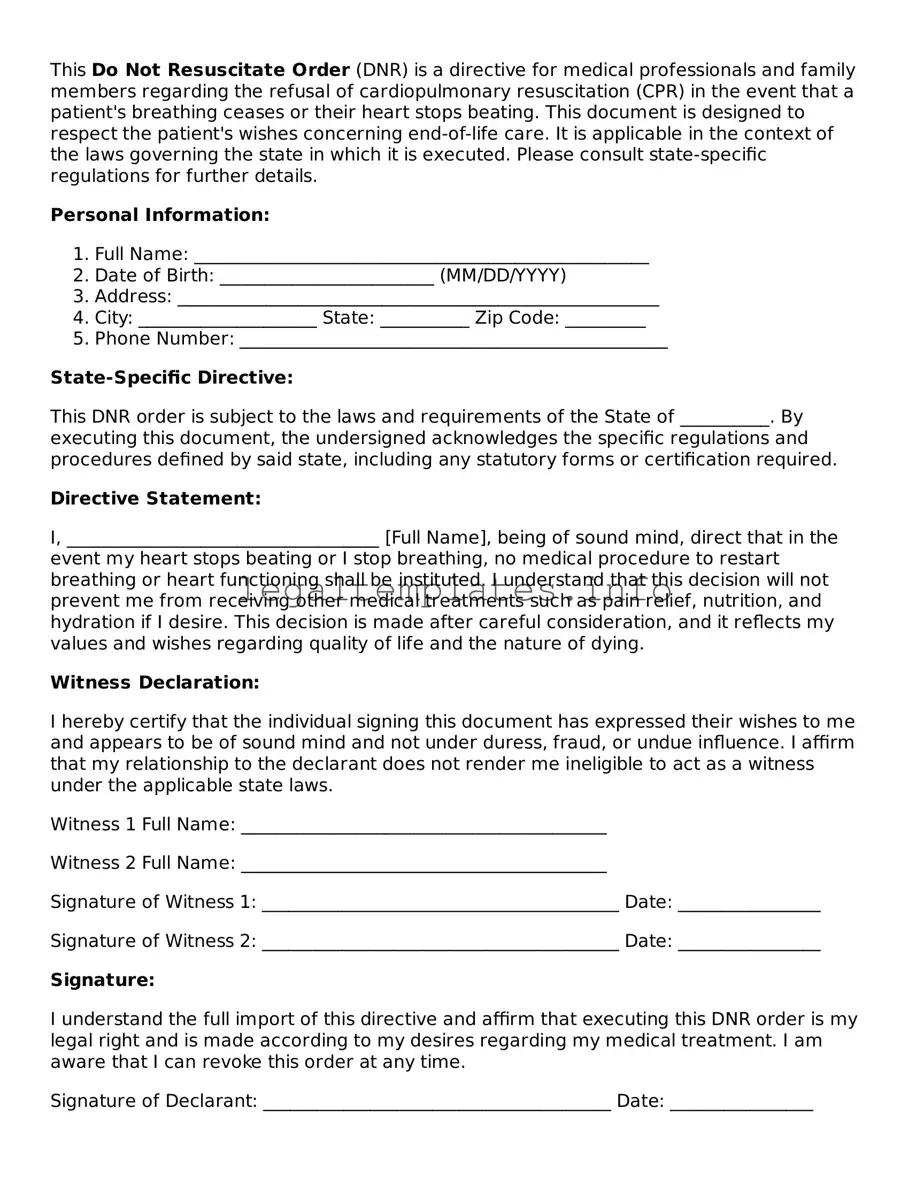
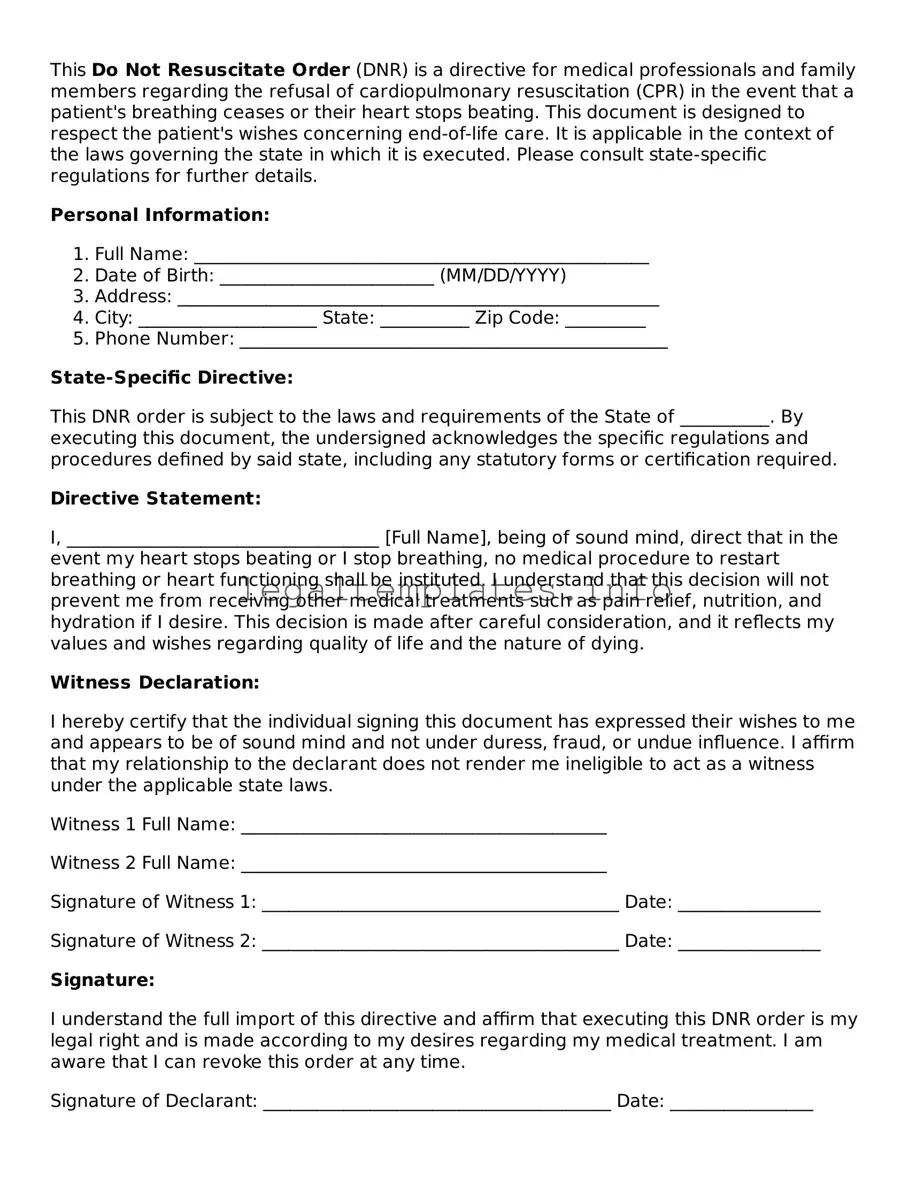
This Do Not Resuscitate Order (DNR) is a directive for medical professionals and family members regarding the refusal of cardiopulmonary resuscitation (CPR) in the event that a patient's breathing ceases or their heart stops beating. This document is designed to respect the patient's wishes concerning end-of-life care. It is applicable in the context of the laws governing the state in which it is executed. Please consult state-specific regulations for further details.
Personal Information:
- Full Name: ___________________________________________________
- Date of Birth: ________________________ (MM/DD/YYYY)
- Address: ______________________________________________________
- City: ____________________ State: __________ Zip Code: _________
- Phone Number: ________________________________________________
State-Specific Directive:
This DNR order is subject to the laws and requirements of the State of __________. By executing this document, the undersigned acknowledges the specific regulations and procedures defined by said state, including any statutory forms or certification required.
Directive Statement:
I, ___________________________________ [Full Name], being of sound mind, direct that in the event my heart stops beating or I stop breathing, no medical procedure to restart breathing or heart functioning shall be instituted. I understand that this decision will not prevent me from receiving other medical treatments such as pain relief, nutrition, and hydration if I desire. This decision is made after careful consideration, and it reflects my values and wishes regarding quality of life and the nature of dying.
Witness Declaration:
I hereby certify that the individual signing this document has expressed their wishes to me and appears to be of sound mind and not under duress, fraud, or undue influence. I affirm that my relationship to the declarant does not render me ineligible to act as a witness under the applicable state laws.
Witness 1 Full Name: _________________________________________
Witness 2 Full Name: _________________________________________
Signature of Witness 1: ________________________________________ Date: ________________
Signature of Witness 2: ________________________________________ Date: ________________
Signature:
I understand the full import of this directive and affirm that executing this DNR order is my legal right and is made according to my desires regarding my medical treatment. I am aware that I can revoke this order at any time.
Signature of Declarant: _______________________________________ Date: ________________
Physician Acknowledgment:
This document has been discussed with the declarant, and I am satisfied that the patient/declarant understands the nature, import, and implications of their decision.
Physician's Name: _____________________________________________
Signature of Physician: ________________________________________ Date: ________________
License Number: ______________________________________________