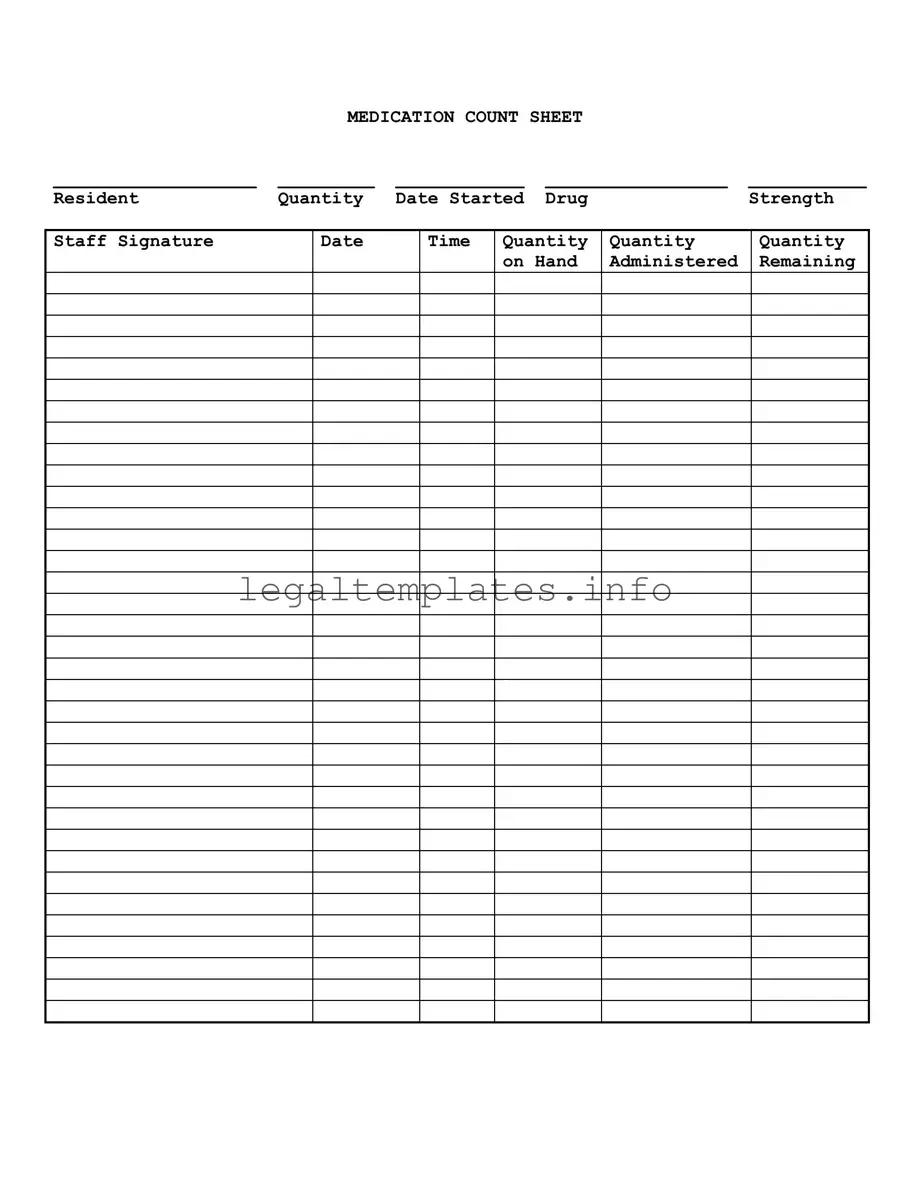
When it comes to managing medication for residents in various settings, the Medication Count Sheet plays a crucial role in ensuring accuracy and accountability. However, there are common pitfalls that can lead to errors in medication management. Understanding these mistakes can greatly improve the effectiveness of medication tracking and administration.
One common mistake is not double-checking the resident's name when filling out the form. This may seem like a basic step, but in busy settings, it's easy to mix up sheets or overlook discrepancies. This can lead to administering medication to the wrong resident, which is both dangerous and a violation of trust.
Another error is incorrectly recording the quantity of medication on hand at the start. This initial count is the foundation for all future entries on the sheet, and inaccuracies can cascade, leading to confusion about whether medications have been administered properly or even prompting concerns about medication security.
Often, staff may rush and forget to record the date and time when medication is administered. This oversight can complicate efforts to track when the last dose was given, which is especially critical for medications that must be spaced out precisely to maintain their effectiveness.
A lack of consistency in how the staff signature is recorded is yet another mistake. Inconsistent or missing signatures make it difficult to verify who administered medication, complicating accountability and potentially hindering follow-up in case of an adverse reaction or other issues.
Failing to accurately note the quantity of medication administered is a significant error. Whether it's giving too much, too little, or failing to record the dose accurately, such mistakes can have serious health implications for residents and legal ramifications for the facility.
Not updating the quantity remaining after each administration is a critical oversight. This information is essential for knowing when to reorder medication and for preventing either stock-outs or overstocking, which can lead to medication wastage or misuse.
Omitting or incorrectly filling out the drug strength field can lead to errors in medication administration, especially in settings where a medication comes in multiple strengths. Administering the wrong strength of a medication can have substantial consequences for patient health.
Ignoring or inaccurately tracking the date the medication was started is yet another common error. This information is pivotal for determining the course of treatment and ensuring that medication is administered within its effective date range and discontinued appropriately.
Last but not least, a simple yet impactful mistake is the failure to regularly review and reconcile the Medication Count Sheet with the actual medication stock. Regular checks can prevent many of the aforementioned errors from becoming problematic, ensuring both the health and safety of the resident and regulatory compliance for the facility.
By being mindful of these common mistakes and taking steps to avoid them, staff can greatly improve the accuracy and reliability of medication administration, ultimately ensuring better care for their residents.