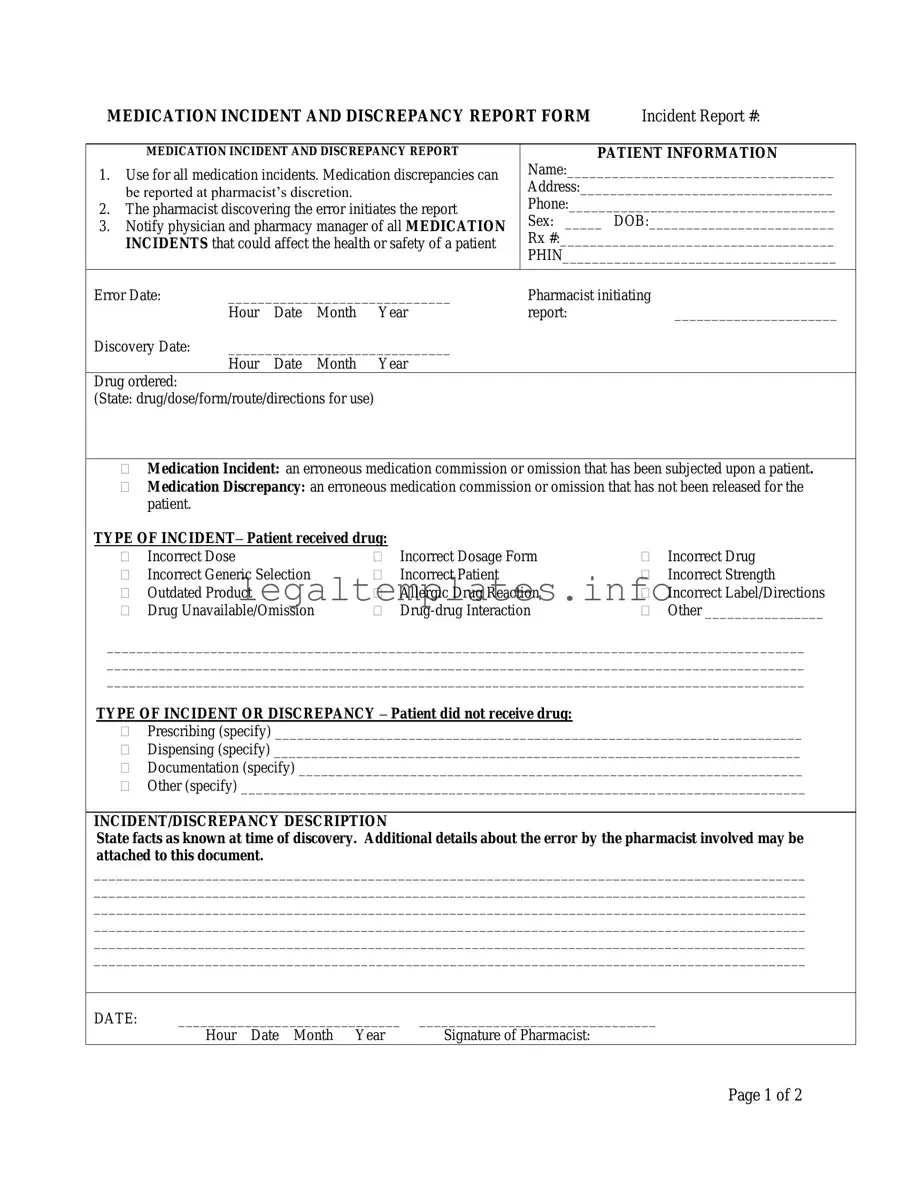
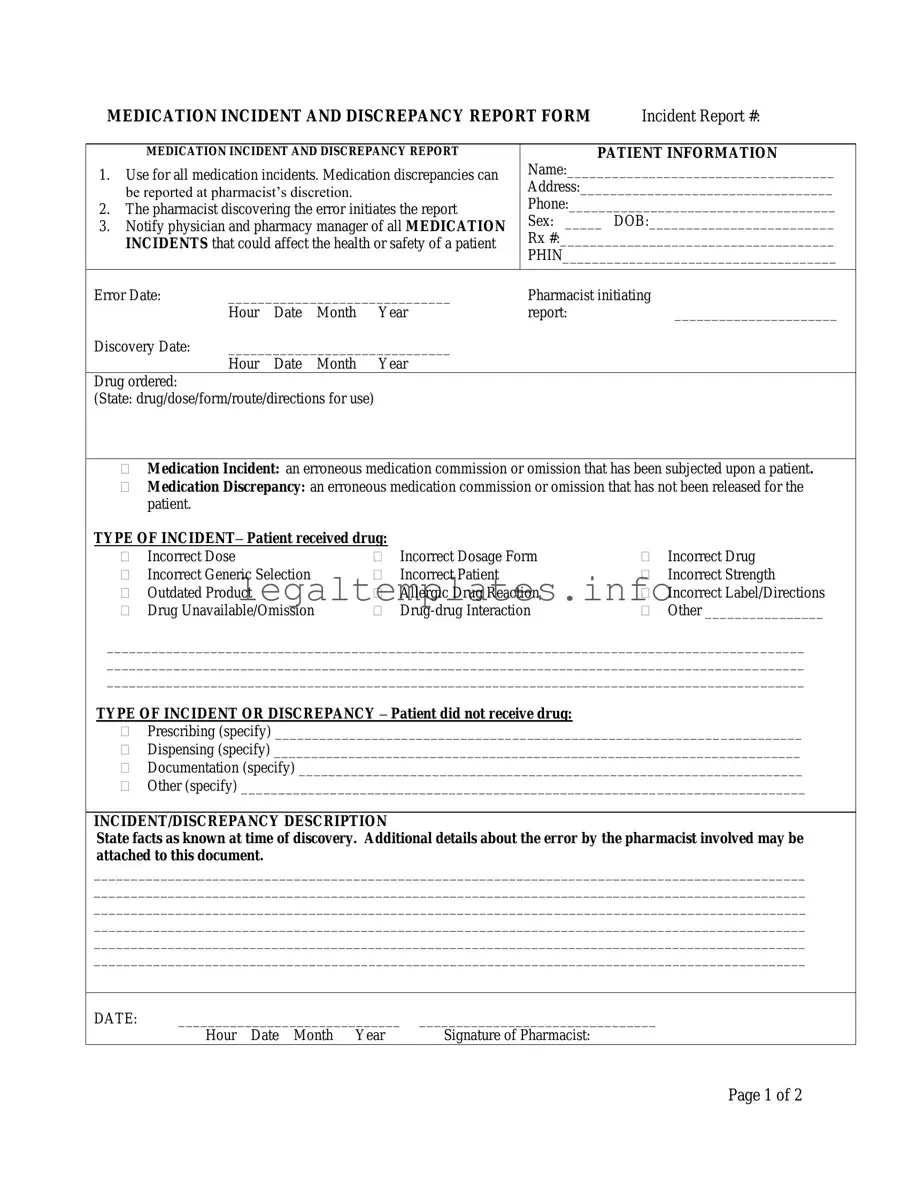
The Medication Error form bears a strong resemblance to a Patient Safety Incident Report often found in hospitals and healthcare settings. Both documents are designed to capture detailed information about events that compromise the safety or health of patients. Like the Medication Error form, the Patient Safety Incident Report includes sections for describing the incident, the individuals involved, the date and time of occurrence, and any immediate actions taken. However, while the Medication Error form focuses specifically on medication-related incidents, the Patient Safety Incident Report covers a broader range of safety incidents, including falls, procedural mistakes, or equipment failures.
Another document similar to the Medication Error form is the Adverse Drug Reaction (ADR) Report. Both forms are used to document undesirable experiences associated with the use of a medicinal product. The ADR Report, much like the Medication Error form, collects details on the drug involved, patient information, the nature of the adverse reaction, and the outcome. The key difference lies in their focus: the Medication Error form documents errors in the medication process, whether or not harm occurred, while ADR Reports specifically document harmful reactions that are linked to the pharmacological action of the medicine.
A Quality Assurance (QA) Incident Report, used in various industries including pharmacy and healthcare, also shares similarities with the Medication Error form. QA Incident Reports aim to document any deviation from standard procedures or expectations, analyzing and addressing the root cause to improve quality and safety. Both this form and the Medication Error form include sections for incident description, involved individuals, and resolution actions. However, QA Incident Reports are broader in scope, potentially covering non-medical incidents as well.
Medication Administration Records (MAR) share some characteristics with the Medication Error form, primarily in their detail on drug administration. While MARs are used to record all medications administered to a patient, noting the time, dose, and person who administered it, the Medication Error form is invoked only when discrepancies or incidents occur in the medication process. Both serve as crucial documentation for ensuring patient safety and effective medication management, but the Medication Error form serves specifically as a tool for error reporting and prevention.
The Near Miss Report is another document related to the Medication Error form. A near miss in healthcare is an event that could have led to an adverse patient outcome but did not, either by chance or timely intervention. Both forms collect information on the incident details, individuals involved, and the steps taken to resolve the issue. The key difference is that the Near Miss Report focuses on incidents without actual harm, highlighting potential vulnerabilities that need attention to prevent future errors.
Clinical Trial Adverse Event Reporting Forms share a similar purpose with the Medication Error form in the context of research studies. These forms are used to document any adverse events experienced by participants during a clinical trial. Like the Medication Error form, they include detailed information on the event, drug involved, and patient details. The principal distinction is their context of use: clinical trials versus routine healthcare service delivery.
Drug Recall Forms similarly focus on medication-related issues, specifically for documenting and managing the process of recalling faulty or dangerous medicinal products. They collect data about the product, the reason for the recall, and actions taken. While the Medication Error form is used to document errors that have occurred at the point of care, Drug Recall Forms serve a broader purpose in public health safety, managing the withdrawal of products from the market to prevent harm.
The Patient Complaint Form, often used in healthcare settings, overlaps with the Medication Error form in its function to capture feedback on service delivery issues. While the Patient Complaint Form can cover a wide range of issues from rudeness to delays in service, it can also include complaints related to medication errors, making both forms integral to quality improvement efforts. The key difference lies in their initiation: one is filled out by healthcare professionals post-incident, and the other by patients or their families.
Finally, the Healthcare Audit Forms, used to systematically review and assess the quality and safety of clinical care, including medication management practices, also resemble the Medication Error form in some aspects. Though Audit Forms are used in a more proactive approach to prevent medication errors by identifying lapses in protocols or practices, they can highlight the same types of medication discrepancies or incidents post-factum, aiming for systemic improvements rather than addressing individual occurrences.