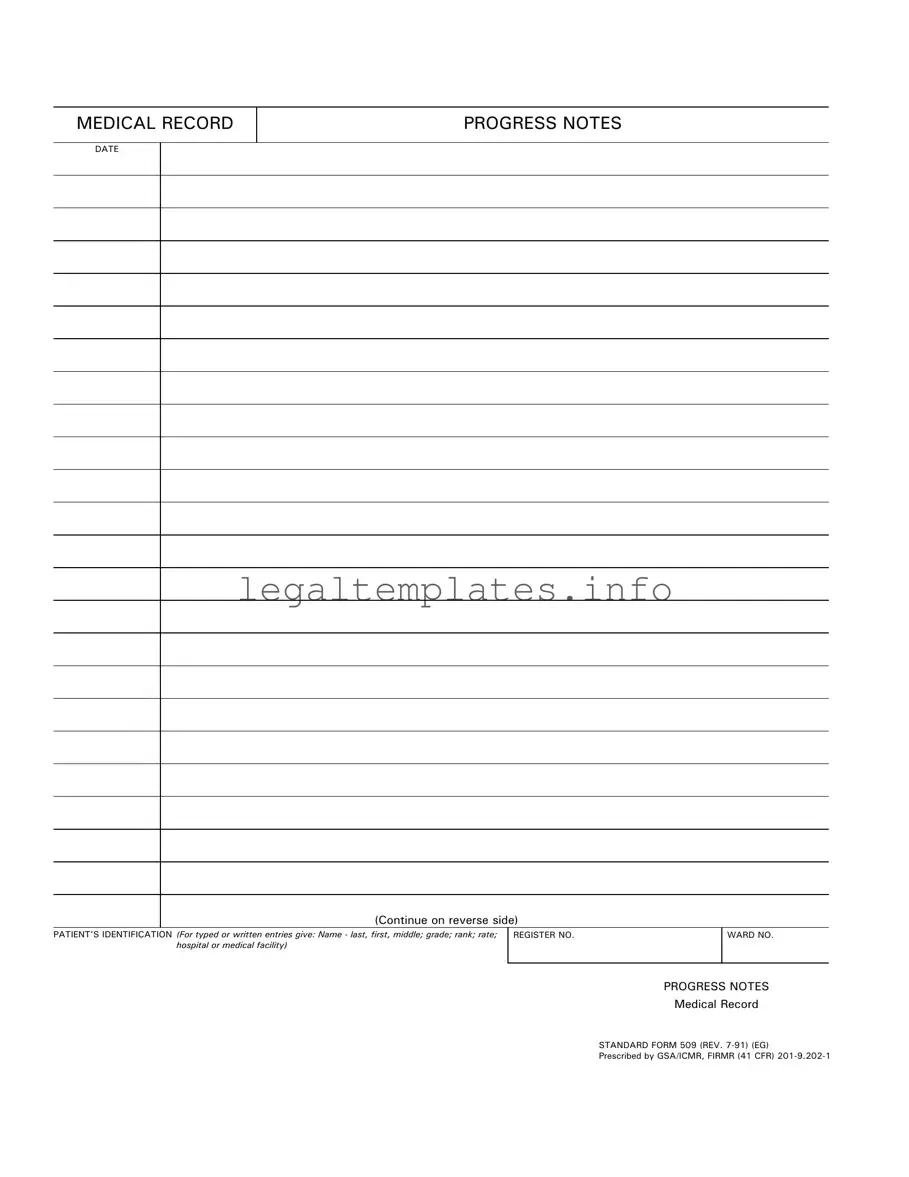
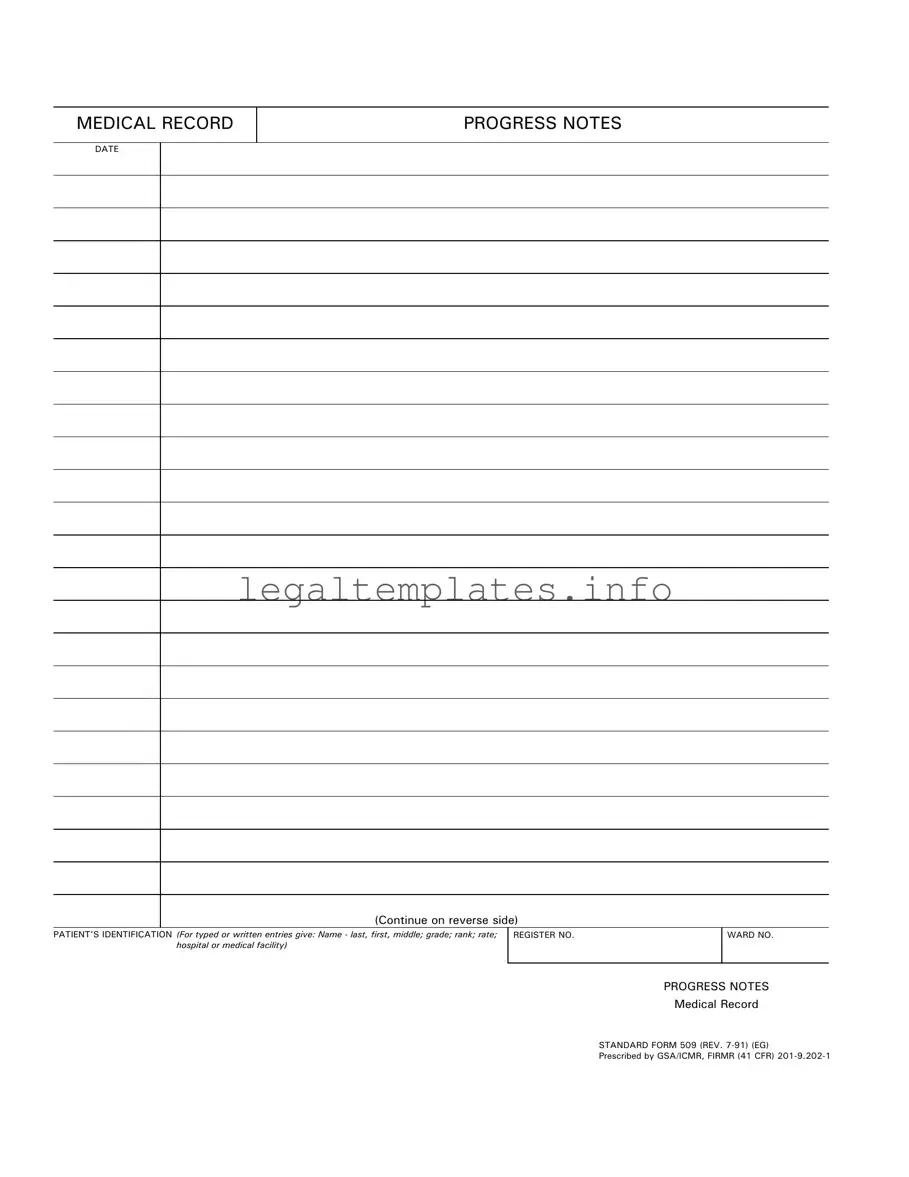
What are Progress Notes?
Progress Notes are detailed records made by healthcare providers during the course of treatment for a patient. These notes include observations, treatment details, responses to treatments, and the evolving status of the patient's health. The information is chronologically ordered, making it easier to track the patient's progress over time.
How do I fill out the Patient's Identification section on a Progress Notes form?
For the Patient's Identification section, you need to provide comprehensive details about the patient. This includes the patient’s name – starting with the last name, followed by the first and middle names. You should also write the patient’s grade, rank, rate, and the hospital or medical facility where they are receiving care. Don’t forget the patient’s register number and ward number, if applicable.
What should be included in the Progress Notes?
In the Progress Notes, healthcare providers should include all observations related to the patient's condition, any treatments administered, and the patient's responses to those treatments. It's also important to note any changes in the patient’s condition, whether they are improvements or deteriorations. These notes should be detailed and objective, providing a clear picture of the patient's journey through care.
Can Progress Notes be continued on another sheet?
Yes, if the space provided on the front side of the Standard Form 509 is insufficient, the notes can be continued on the reverse side of the form. If more space is needed beyond that, additional sheets can be attached, ensuring that patient identification details are clearly marked on each page to maintain continuity and prevent any mix-up of records.
Who can write in the Progress Notes?
Authorized healthcare providers caring for the patient are the only individuals allowed to make entries in the Progress Notes. This includes doctors, nurses, therapists, and other medical professionals directly involved in the treatment and observation of the patient. Each entry must be signed by the person making it, along with their title or role.
Is there a specific format for writing dates in Progress Notes?
Yes, when making entries in the Progress Notes, it's crucial to follow the established format for dates to ensure clarity and consistency across medical records. The Standard Form 509 specifies the use of the REV. 7-91 format, but always check for any updated guidelines from the hospital or medical facility to ensure compliance with current standards.
Why is it important to fill out the Progress Notes accurately?
Accurately filled Progress Notes are vital for several reasons. They provide a comprehensive history of the patient’s treatment and condition over time, which is crucial for continuity of care, especially when different healthcare providers are involved. They also serve as legal documents that may be reviewed in case of disputes or inquiries about the patient's treatment. Finally, they are essential for auditing and quality control within the healthcare facility.
How is patient confidentiality protected with Progress Notes?
Patient confidentiality is protected by adhering to strict guidelines for storing, handling, and sharing Progress Notes. Only authorized personnel are allowed access to these records. When transferring notes or making them available to other parts of the healthcare system, all necessary precautions are taken to ensure that patient information is shared securely and only with those who have a legitimate need to know for the purpose of continued care or treatment.