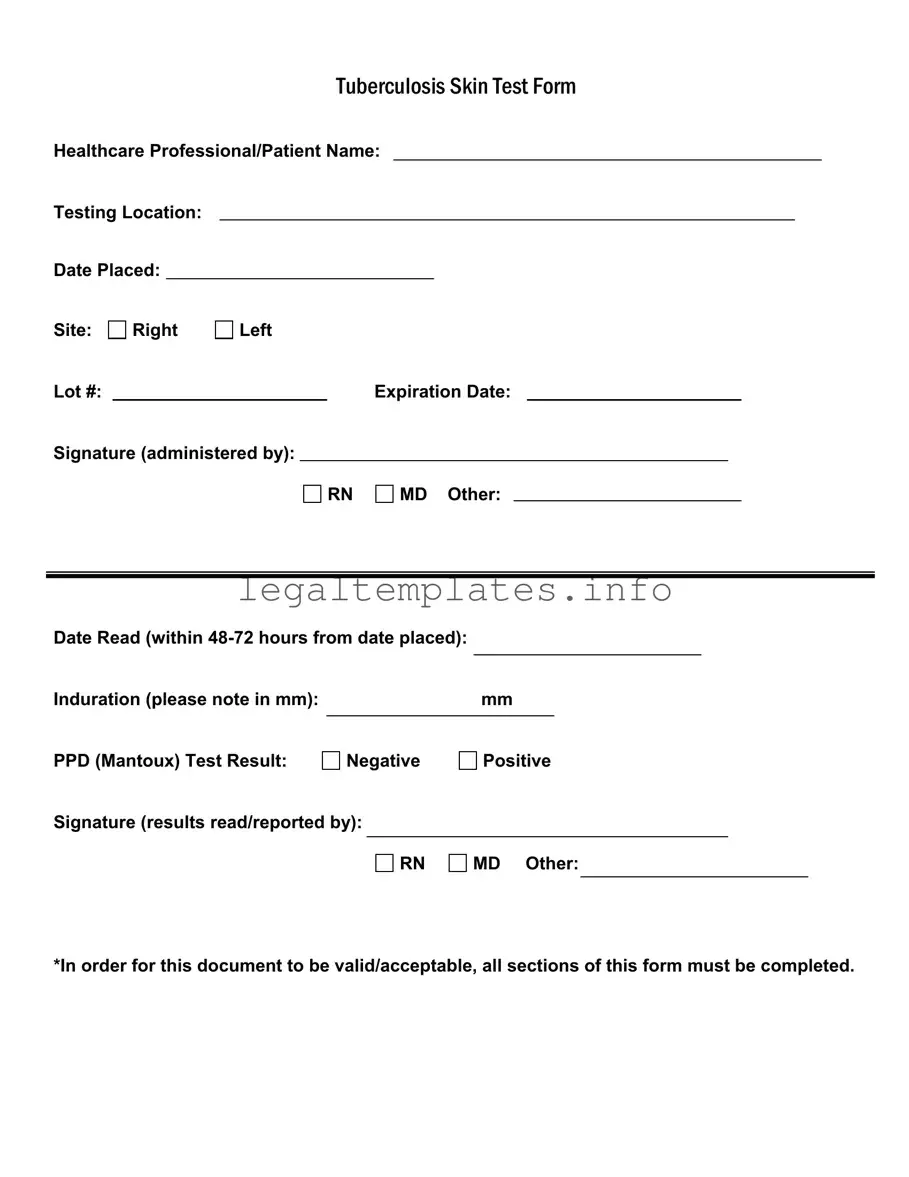
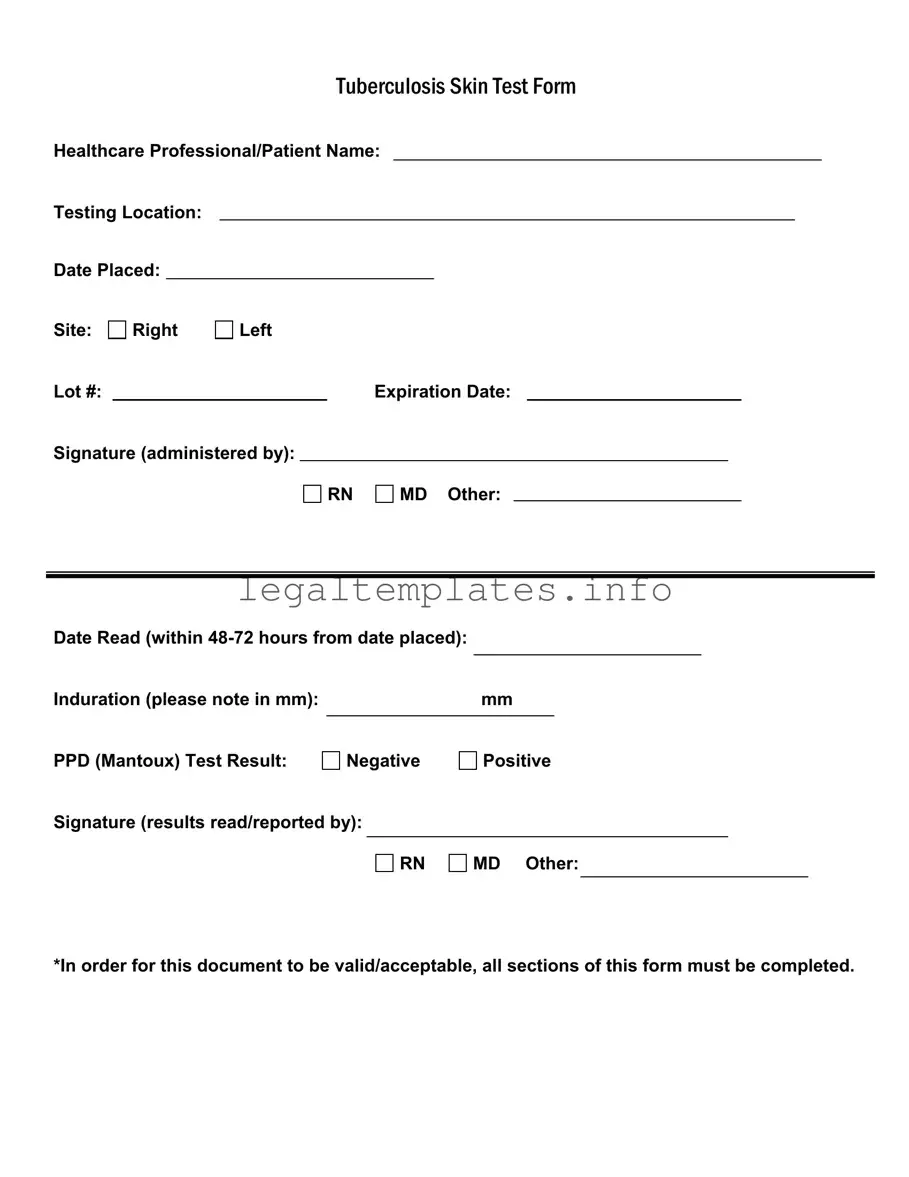
What is a Tuberculosis (TB) Skin Test Form?
This is a document used by healthcare professionals to record the details and results of a Tuberculosis skin test, also known as the Mantoux test. The form captures information about the patient, test administration, and the outcomes, ensuring a clear record for follow-up and treatment if necessary.
Who can administer the TB skin test?
The TB skin test should be administered by a qualified healthcare professional. This includes Registered Nurses (RN), Medical Doctors (MD), or other certified practitioners authorized to perform this procedure.
What does the testing location refer to on the form?
The testing location indicates the facility or specific area where the TB test is conducted. This could be a hospital, clinic, or any healthcare setting equipped to perform TB skin testing.
Why is there a section for the site of the test (Right or Left)?
This section refers to the arm on which the test is administered. Indicating whether the right or left arm was used helps in tracking and assessing the test results accurately, especially if multiple tests are needed over time.
What is the significance of the lot number and expiration date on the TB Test Form?
The lot number and expiration date relate to the Tuberculin skin test solution used for the test. This information is crucial for tracking the vaccine batch and ensuring its effectiveness at the time of administration.
What does it mean by induration noted in mm?
Induration refers to the raised, hardened area that may appear at the test site after 48-72 hours. Measuring its size in millimeters (mm) helps healthcare professionals determine the result of the test. A specific size may indicate a positive reaction.
How is the test result determined as negative or positive?
The PPD (Mantoux) Test Result is categorized as negative or positive based on the size of the induration. Specific criteria, such as the individual’s risk factors and the mm size of the induration, are considered to interpret the results.
Who should read and sign off on the test results?
A qualified healthcare professional, such as an RN, MD, or authorized provider, must read and interpret the results. The same or another qualified individual must then sign off on the form to validate its accuracy.
Why is it necessary for all sections of the TB Test Form to be completed?
Completing all sections ensures the form is legally and medically valid. It captures essential details for accurate record-keeping, follow-up, and if required, treatment initiation. Incomplete forms may not provide sufficient evidence of test administration or results.